The Liver Unit of the Department of Surgery at the Milan University, Italy, published in September's issue of HPB journal a study which aimed at determining wether steroid administration may reduce liver injury and improve short term outcome.
The study included 43 patients undergoing liver resection, randomizing the groups to steroid receiving patients and a control group. Patients receiving steroids, were given 500 mg of methylprednisolone preoperatively. Levels of ALT, AST, total bilirubin, AT-III, PT, IL-6, TNF alfa were compared. Length of stay and complications were recorded.
Postoperative serum levels of ALT,AST, total bilirubin, inflammatory cytokines were lower in the steroid group. The incidence of postoperative complications in the control group tended to be higher than the steroid group.
The study concluded that steroid pretreatment represents a potentially important biologic modifier of I/R injury and may contribute to maintenance of coagulant/anticoagulant homeostasis.
Print Post
2007/10/13
Randomized Study of the Benefits of Preoperative Cosrticosteroid Administration on Hepatic I/R Injury
Posted by Dr. E Flores Rivera at 11:49 AM 0 comments
Labels: hepatectomy, ischemia, liver, milan, reperfusion, steroids, study, surgery
2007/10/10
Surgical Techniques for Liver Transection
Liver resection is still a surgical challenge, due to the high risk of hemorrhage during the transection and the complicated biliary and vascular anatomy of the organ.
The history of the development of surgical techniques for liver resection had it’s main goal, the fight against bleeding. Before 1980’s, liver resection was associated to 10-20% mortality rates.
Currently the in hospital mortality nears 5% in specialized centers. Even though there is a better patient selection, the reduction in blood loss and perioperative transfusions have contributed to the better patient survival. Massive bleeding and transusions not only rise the morbi-mortality risk, but also compromise long term survival after resection of liver tumors, due to the associated immunesuppression, which leads to recurrence.
Finger fracture of the liver parenchyma has been the classic technique for liver resection. During the last 20 years, technological advances have lead to the development of specific instruments such as the compact ultrasonic surgical aspirator, water jet, harmonic scalpel, Ligasure®, and TissuLink®. Another thing that has reduced intraoperative blood loss is the better delineation of the transection plane with the use of IOUS.
Delineation of the Proper Transection Plane
This is not only important to achieve an adequate margin for resection of liver tumors, but also to avoid inadvertent injuries to major hepatic vessels or ducts.
This delineation starts with an adequate knowledge of the computed tomography, to define the different relationships of the tumor and the hepatic veins and biliary pedicles. This can be evaluated transoperatively by IOUS.
Without this knowledge inadvertend injuries may occur during transection, which can lead to massive bleeding or biliary injuries. In some occasions tumor exposition during transection can happen. Generally a 1cm margin is required, but this is still controversial for HCC (Ann Surg 2000; 231: 544-551).
IOUS allows localization of the portal pedicle of each liver segment. Some surgeons perform the liver tattoing with blue dye, injected directly to one portal branch to delineate the segment that is going to be resected.
Techniques of Liver Transection
Finger fracture/clamp crushing
Vacular control is very important to hepatobiliary surgeons. Transection is particularly difficult in cirrhotic livers due to fibrosis. The risk of bleeding is also high in this pathology.
Finger fracture involves crushing the liver parenchyma while under inflow occlusion. This technique was introduced by Lin in 1958 (J Formosa Med Assoc 1958; 57: 742-749). Subsequently was perfected by the introduction of other instruments such as the Kelly clamp (Ann Surg 1974; 180: 285-290). Currently is one of the most widely used techniques today.
Ultrasonic Dissection
In a lot of centers, the use of Cavitron® CUSA (Compact Ultrasonic Surgical Aspirator) has been the standard for liver resection. With this technology, liver parenchyma is fragmented by means of ultrasonic energy and aspirated exposing the vascular and ductal structures, which can be clipped or ligated.
This technique has demonstrated reduction in blood loss, morbidity, when compared with finger crushing. The surgical margin is also wider with this technique (Br J Surg 1996; 83: 117-120).
Water Jet
The water propulsion dissector uses a water jet instead of ultrasonic energy to fragment liver parenchyma and expose vascular and biliary structures. This technique is not as popular as CUSA. Currently only one study showed the results with this technique (Zentralbl Chir 2001; 126: 586-590).
Harmonic Scalpel
More recently, newer technologies have allowed sealing of lesser vessels during liver transection. This technique can be used alone or in conjuction with others, such as finger crushing or CUSA.
It uses ultrasonicaly activated shears to seal small vessels that stand between the vibrating blades. The blades vibrate at 55.5 kHz and can easily dissect parenchyma. The coagulative effect is caused by protein denaturalization that occurs due to destruction of hydrogen bonds and heat generation. The tissue cutting effect derives from a saw mechanism.
It has been used in laparoscopic and open procedures, without reported biliary leaks in Schmidbaier’s study in 2002 (Ann Surg 2002; 235: 27-30).
One disadvantage of this technique is it’s capacity to dissect the liver parenchyma around the hepatic veins, because of its difficulty in controlin large vessels. Even though, it is widely used in laparoscopy.
Ligasure
Another instrumet designed for sealing small vessels using a different principle. Combining compression and bipolar radiofrequency energy, a change in the vessel wall’s collagen and elastin, sealing of vessels as large as 7 mm can be achieved.
Doubts concernig its capacity of sealing large bile ducts persist, and ths was reafirmed in a recent study (World J Surg 2005; 29: 110-112). It is useful for laparoscopic procedures.
TissueLink
A new technology using saline-linked radiofrequency energy has been developed. The saline runs towards the tip of the instrument to link the radiofrequency energy with liver surface, achieving coagulation.
This instrument has a tip that allows transection and vessel sealing simultaneously. Can be used during laparoscopic surgery. You can watch a video here.
Radiofrequency Assisted Liver Transection
Radiofrequency ablation is a good technoque for the treatment of liver tumors. With this technique, a Cool-tip® electrode is inserted in the transection plane serially every 1-2 cm, applying energy for 1-2 minutes, to create coagulated cylinders, that then can be cut by a scalpel.
The advantage of this technique is its simplicity, when compared to the other techniques. One of the potential disadvantages is the sacrifice of liver prenchyma that is coagulated, leaving up to 1 cm of necrotic tissue, which can be critical in cirrhotic patients.
There exists the concern for damage to the hilar structures and hepati veins. The use of this device has to be evaluated. You can watch a video here.
Print Post
Posted by Dr. E Flores Rivera at 8:45 PM 0 comments
Labels: cusa, finger crushing, habib sealer, harmonic scalpel, ligasure, liver, liver transection, surgery, tissuelink
2007/10/06
Surgical Management of Colorectal Liver Metastases
The appearance of liver metastases during the evolution of a primary colorectal tumor is a bad prognosis. To prolong the patient's life, many therapies have been proposed, more importantly, chemotherapy.
Today, surgical resection is the only therapeutic option for cure, and attains survival curves at medium and long term, superior to those obtained by other treatments. Resection achieves survival rates of 26 to 45% at 5 years, while it is almost zero in those cases not resected.
Liver resection leads to low morbidity and mortality, close to 1% in specialized centers. It must be emphasized that out of all the patients with colorectal liver metastases, only 10 to 20% can be resected. Today, the challenge is to develop new startegies thatt combine surgical resection with techniques of tumor destruction such as RFA, cryotherapy, portal embolization, and new chemotherapy protocols, with the goal of making those lesions that are initially considered unresectable, resectable.
Principles of Curative Liver Resection
The techniques are divided into 'anatomical' or 'non-anatomical' resections.
Anatomical Resections
They follow the liver segmentation principles described by Couinaud. They are considered as minor, when less than 3 segments are resected, or major, when resection inludes more than 3 segments.
Non-Anatomical Resections
They include the resection of a portion of the liver independently of the liver scisures and glissonian pedicles. They refer mainly to metastasectomies. The liver resection depends on the size of the tumor.
Rules to Respect During Hepatectomy
Independently of the type of liver resection, one must follow these rules in order to avoid postoperative complications:
* Functional liver parenchyma preservation of at least 30% of the total liver mass, to avoid hepatic insufficiency.
* Limit blood loss, in order to avoid transfusions, because it is a known risk factor that favors recurrence.
* Respect the 1 mm margin, to reduce the risk of recurrence.
* Respecto glissonian pedicles destined to the remaining segments, to avoid segmental exclusion, ischemia and necrosis, and biliary fistulas.
Preoperative Patient Evaluation
Before even thinking on performing a liver resection, it is necessary a thorough oncologic examination, seeking other localizations, and also to verify the absence of contra-indications.
Regarding morphological tests, an abdominal US, CT and afterwards a MRI, allow to acquire a better knowledge regarding number of metastases, precise location, relationship with the portal pedicle and the hepatic veins.
Pulmonary localizations must be ruled out systematically, using CT examination. If these lesions are resectable, they dont constitute a contraindication to liver resection. The same goes for all of the extrahepatic metastases.
A colonoscopy is always performed to rule out recurrence, even if the primary tumor has already been resected. If necessary, a bone scan or a brain CT can be performed.
Regarding the blood chemistry, it consists of liver function tests, tumor markers, coagulation profile and clearance of green indocyanine test, which allows to better evaluate liver function, specially in those patients who received neoafjuvant chemotherapy or those with a preexistent liver pathology (hepatitis, cirrhosis).
Valid Indications and New Operative Strategies
A patient with liver metastases limited to one segment without extrahepatic dissemination is always a candidate for liver resection. The challenge for hepatobiliary surgeons is to achieve the necessary resources and strategies that allow the patients' benefit.
The liver surgical progress and the development of new surgical techniques, like RFA, cryotherapy, new radiological interventions such as portal embolization, and new chemotherapy drugs have permitted the elaboration of this new strategies, which make possible curative resections to patients initially considered unresectable. Patients can be divided into four groups:
1. Patients with a voluminous hepatic metastases in which resection leaves an insufficient amount of functional liver parenchyma.
2. Patients with bilobar metastases.
3. Patients with recurrence after resection.
4. Patients with a primary colorectal tumor and synchronous liver metastases.
Patients with a Voluminous Liver Metastases
Two alternative may be offered: Tumor downsizing with systemic or local chemotherapy, and hypertrophy of the future remaining liver (non-tumoral) by portal embolization.
* Downsizing: Bismuth et al, from the Paul Brousse Hospital in France, showed in a study with 53 patients presenting with liver metastases initially non-resectable, that the use of neoadjuvant chemotherapy with 5-fluorouracyl, folinic acid and oxalyplatin, achieved an adequate tumoral downsizing, with similar results as those patients initially resectable. (Ann Surg 1996; 224: 509-522).
* Portal Embolization: When resection is not viable due to insufficient functional liver parenchyma (usually left lobe), surgeons look for hypertrophy of the non-tumoral liver. Once embolization is performed, hypertrophy is evaluated 5-6 weeks after the procedure. If the future remaining liver is >30%, then hepatectomy can be performed.
Patients with Bilobar Metastases
Many therapeutic options have been described:
* Two-stage Hepatectomy including Portal Embolization: The success seen for one stage hepatectomies after portal embolization, lead surgeons to the two stage procedure. This strategy consists on a first stage of metastases resection in the future remnant, and embolization of the tumoral liver. On a second stage, a right hepatectomy is performed, which can be extended to segment 4, after an adequate hypertrophy is achieved.
* Two-stage Hepatectomy: Described by René Adam, consists on the resction of the majority of the metastases in a first stage. Then resection of the remaining lesions after acquiring liver regeneration. In between, patients receive chemotherapy.
* Hepatectomy associated to resection and tumoral destruction by local treatment: Here, the greater lesions are resected and the lesser ones are destroyed locally by either RFA or cryotherapy.
* Two-stage Hepatectomy after neoadjuvant chemotherapy: The goal is to achieve an adequate downsizing of the tumor that allows for a resection in a one-stage or two-stage procedure.
Patients with Recurrence after Resection
Surgery is the only curative option for these patients. It has been shown that patients with a liver recurrence isolated or associated with a resectable extrahepatic metastases, resection of all the tumoral tissue achieves an overall survival similar to patients without recurrence.
Resection of the recurrence turns the clock back to zero. In these cases, tumor destruction by RFA or cryotherapy extends the indications.
Patients with a Primary Colorectal Tumor and Synchronous Metastases
Surgical startegies remain controversial. Those who favor simultaneous resection, and those who oppose it, differ in terms of oncological basis, immunological techniques and patient comfort. Jaeck showed that there was no difference between the two approaches (Chirurgie 1999; 124: 258-263).
Print Post
Posted by Dr. E Flores Rivera at 11:35 AM 0 comments
Labels: bismuth, colorectal cancer, cryotherpy, jaeck, liver, liver metastases, portal embolization, radiofrequency, RFA, surgery
2007/10/01
ESOT: Extra-Small-For-Size Grafts In Living Donor Liver Transplantation
Dr. Yuji Seojima of the Kyushu University, Fukuoka, Japan presented today his study regarding ESFS grafts.
Among their 244 LDLT (71 right lobe and 143 LL), 15 were less than 30% of the graft-to-standard liver volume ratio. All of the ESFSG were left lobe grafts. The mean graft weight was 301 grams.
Several technical modifications were necessary such as: AOLT (n=2), temporal hemiportocaval shunt (n=1), splenectomy (n=1). Four grafts were lost to chronic rejection, late portal vein thrombosis, de novo lung cancer, and hepatic infarction.
They concluded that the ESFSG can be used safely in selected cases with appropiate technical modifications, careful patient management and the accumulation of experience.
Print Post Read More......
Posted by Dr. E Flores Rivera at 6:41 PM 0 comments
Labels: dual grafts, ESOT, extra small for size grafts, heart transplantation, japan, liver
ESOT: Adult-To-Adult Living Donor Liver Transplantation Using Dual Grafts
Dr. Chih-Chi Wang from the Department of Surgery at Kaohsiung Hospital, Taiwan, presented at the ESOT Congress, Prague, their experience with dual grafts for living donor liver transplantation.
They presented a prospective study including 150 adult LDLT and 5 dual graft transplantations. According to their results, 2 recipients received 1 right lobe and 1 left lobe, and the other two received two left lobes.
They concluded that dual graft transplantation provides sufficient volume in the recipient without jeopardizing donor safety. They also added that it should be considered and performed by an experienced center when a single donor is rejected based on volumetry requirements.
Print Post
Posted by Dr. E Flores Rivera at 2:23 PM 0 comments
Labels: dual grafts, ESOT, LDLT, liver, liver transplantation, surgery
2006/10/27
Solitary Colorectal Liver Metastases
 This study comes out from the M.D Anderson Cancer Center. The aim was to compare Liver resection to Radiofrequency ablation in the treatment of colorectal liver metastases (CRLM). I think it is a very interesting study, because it embraces what other previous studies have been showing, this is, that overall survival has been increasing with hepatic resection in patients with CRLM.
This study comes out from the M.D Anderson Cancer Center. The aim was to compare Liver resection to Radiofrequency ablation in the treatment of colorectal liver metastases (CRLM). I think it is a very interesting study, because it embraces what other previous studies have been showing, this is, that overall survival has been increasing with hepatic resection in patients with CRLM.They concluded that The survival rate following HR of solitary colorectal liver metastasis exceeds 70% at 5 years. Radiofrequency ablation for solitary metastasis is associated with a markedly higher LR rate and shorter recurrence-free and overall survival rates compared with HR, even when small lesions ( 3 cm) are considered.
ARCHIVES OF SURGERY. VOL 141, MAY 2006.
Posted by Dr. E Flores Rivera at 2:44 PM 0 comments
Labels: cancer, colorectal, liver, metastasis
2006/10/25
Liver transplantation and Immunosuppression
The early 1970s saw the introduction of a new class of immunosuppressants, the so-called “calcineurin inhibitors” (CNIs). These compounds form the backbone of immunosuppression in liver transplantation recipients. Currently, two CNIs are available: Cyclosporine A and Tacrolimus (TAC).
CyA was discovered by Jean-Francois Borel in 1973 from a soil fungus, Tolypocladium inflatum. Food and Drug Administration approval was obtained in 1983. CyA causes selective suppression of cell-mediated immunity via inhibition of T-cell activation. After forming a complex with its cytoplasmic receptor protein (cyclophilin), CyA binds to and inhibits the calcium and calmodulin-dependent phosphatase calcineurin. It is believed that calcineurin plays a vital role in the transcriptional process by which interleukin (IL) 2 and other cytokines are activated. The production of these substances by T helper cells is a vital component of the immune response and is central to the graft rejection process.
Nephrotoxicity is one of the main side effects of CyA therapy. This can be both an acute and a longterm complication, inducing a post-OLT rate of renal failure up to 20%.Common metabolic abnormalities include hyperkalemia, hypomagnesemia, hyperlipidemia, and, to a lesser extent, hyperglycemia. Hypertension, gingival hyperplasia and hirsutism are also a common occurrence. Between 10% and 28% of patients have neurological manifestations
that range from mild tremor and peripheral neuropathy to psychoses, hallucinations, motor
weakness, and seizures.
In 1984, a soil sample containing the fungus Streptomyces tsukubaensis was discovered from near mount Tsukuba in Japan. Two years after this discovery, TAC was isolated.TAC is 100 times more potent than CyA and exerts its action by binding to FK binding protein (FKBP12).
This complex then inhibits calcineurin, which is responsible for transcription of IL-2, IL-3, IL-4, IL-8, and various chemotactic factors. TAC absorption occurs in the duodenum and jejunum. Unlike CyA, TAC absorption is not influenced by presence of bile, which is advantageous in cholestatic patients or those with biliary diversion or ileus. Food reduces bioavailability, and TAC should be taken on an empty stomach. Metabolism occurs in the liver via the cytochrome P450-3A. Side effects are similar to CyA, including nephrotoxicity, neurotoxicity, posttransplant diabetes mellitus, and hyperkalemia.
Corticosteroids
As mentioned earlier, corticosteroids have been a mainstay since early days of liver transplant. It is by far the most heavily utilized non-calcineurin inhibitor in liver transplant. Corticosteroids exert their most critical immunosuppressive effect by blocking T-cell– derived
and antigen-presenting cell-derived cytokine expression. This includes IL-1, IL-2, IL-3, and IL-6. Corticosteroids continue to be used in reversing acute rejection and in maintenance therapy. Side effects are numerous and include hypertension, hyperglycemia, osteoporosis, hyperlipidemia, increased risk of gastric ulcers, risk of fungal and bacterial infections, and suppression of HPA axis. Raising concern over negative impact of this class of medication in the recurrence of hepatitis C.
Antimetabolites
Azathioprine was the first antimetabolite used in liver transplant but its use has since decreased dramatically over time. Azathioprine is an imidazolyl derivative of mercaptopurine and antagonizes purine metabolism. The result is an inhibition in synthesis of DNA, RNA, and proteins. Current use stands at 5% of U.S. transplant centers. This has been primarily due to the side effect profile, which includes significant myelosuppression and hepatotoxicity.
Mycophenolate mofetil (MMF, CellCept) and mycophenolic acid (MPA, Myfortic) are the most
recent additions to the antimetabolite arena, with MMF approval in 1995 and MPA in 2004. MPA is a delayed-release product in contrast to MMF, which is immediately released. Both formulations inhibit the de novo purine nucleotide synthesis via abrogation of the inosine monophosphate dehydrogenase and the production of guanosine nucleotides. This action leads to a blockage of DNA replication in T and B lymphocytes that are unable to use alternate salvage pathways.
Studies have shown a large variation in MMF pharmacokinetics in liver transplantation related to fluctuations in serum albumin concentrations, changes not seen in the renal transplant population. Liver dysfunction impairs MPA conjugation and prolongs MPA half-life. Furthermore, TAC has been shown to augment the bioavailability of MPA, resulting in higher exposure to MPA (Tables 6A and 6B). The incidence of adverse effects (nausea, gastritis abdominal pain, diarrhea, and neutropenia) requiring dose reduction or withdrawal is high, ranging from 24% to 57%
Antibody Induction
Antibody therapy has been used as a means of delaying the introduction of maintenance therapy and/or helps facilitate the removal of an immunosuppressive agent, particularly corticosteroids. Antibody therapy can be seen as depleting or receptor modulating or both. reiterate, dose reductions are common and in some patients removed completely, especially when combined combined other myelosuppressive medications, such as sirolimus.
Antithymocyte Globulin (ATG)
Polyclonal antilymphocyte antibody preparations are heterologous preparations. Animals (rabbits and horses) are immunized with human T cells and thymocytes. Antisera are then collected. A purified gamma globulin fraction (ATG) is used to reduce the likelihood of serum sickness. The ATG preparations approved by the Food and Drug Administration are ATGAM (of equine origin) and Thymoglobulin (of rabbit origin). These polyclonal preparations are directed at multiple different epitopes on the T cell (CD2, CD3, CD4, CD8, CD28, and the T-cell
receptor) as well as CD16 found on natural killer cells and macrophages. These antibodies cause depletion of T cells by apoptosis, antibody mediated cytolysis and internalization of the cell surface receptors. The biologic effects of the depleting antibodies are profound and last longer than the presence of heterologous antibody. Side effects can include a “first-dose” effect (cytokine release syndrome) and is related to the myriad of cytokines released by these lymphocytes upon their demise. The symptoms typically include fever, chills, tachycardia, gastrointestinal disturbances, bronchospasm, and fluctuations of blood pressure, which all can be ameliorated by pretreatment with corticosteroids, diphenhydramine, and acetaminophen.
Monoclonal Anti–T-Cell Antibodies
Muromonab-CD3 (OKT3) is a murine-derived antibody directed to a specific portion of T cells. It exerts its activity by binding to the CD3 antigen on the surface of T lymphocytes. This binding inactivates the adjacent T-cell receptor, which is critical for activation of T lymphocytes. The end result is a rapid fall in the number of mature lymphocytes. OKT3 was first used in liver transplantation in 1987 for prophylaxis against acute cellular rejection and later to reduce CNI exposure and treatment of steroid-resistant rejection.More recent data has shown a significant drop-off in favor or IL-2 receptor antibodies and polyclonal preparations.
A cytokine-release syndrome is more frequently associated with the first dose as compared to the polyclonal antibody preparations and starts 1-3 hours following administration. Reactions can be quite severe and can range from flulike symptoms (pyrexia, chills, dyspnea, chest pain, and tightness) to severe and lifethreatening shocklike reactions (pulmonary edema).
These symptoms can be mitigated with the administration of a corticosteroid, diphenhydramine, and acetaminophen just prior to dose administration. Reexposure to OKT3 may result in lower efficacy due to antimurine antibodies that may form. In the early transplant period when the incidence of acute cellular rejection was as high as 71% and steroid-resistant rejection was more common, OKT3 was the mainstay in the treatment of steroid-resistant rejection with high salvage rates. Currently, steroid-resistant rejection rates are much lower, thanks to improved immunosuppressive agents and strategies. OKT3 use today is much lower, with many centers preferring treatment regimens for acute cellular rejection to increasing TAC blood levels and then adding corticosteroid boluses if rejection
is still present.
IL-2 Receptor Antibodies
Two products are currently marketed: basiliximab (Simulect) and daclizumab (Zenapax). Daclizumab is a humanized product while basiliximab shows chimeric properties. Both bind to the IL-2R -chain, which is upregulated on the surface of activated T lymphocytes. Immunosuppression is achieved by competitive antagonism of IL-2-induced T-cell proliferation.
Miscellaneous
The following agents are used at different stages in liver transplant, from induction to conversion. Rapamycin Sirolimus (Rapamune, RAP) is a macrocyclic triene antibiotic (structurally related to TAC) with immunosuppressive, antitumor, and antifungal properties, although the latter 2 are not clinically significant. RAP binds to the immunophilin FKBP12 and blocks the response of T- and B-cell activation by cytokines, which prevents cell-cycle progression and proliferation; in contrast, TAC and CyA inhibit the production of cytokines.
Interestingly, although RAP binds to the same immunophilin (FKBP12) as TAC, it has a very different mechanism of action—i.e., blockage of cell-cycle progression at the juncture of G1 and S phase. Because of this, many refer to the binding site for RAP as the “target of RAP.” Multiple serious side effects have limited its use early on in liver transplantation. This includes leukopenia, thrombocytopenia, elevated serum cholesterol and triglyceride levels, anemia, lymphocele, wound dehiscence, and oral ulcerations. The most serious side effect has been the issue of hepatic artery thrombosis and includes the following black box warning in liver transplantation: “The safety and efficacy of Sirolimus (Rapamune) as immunosuppressive therapy have not been established in liver transplant patients, and therefore such use is not recommended.”
Current Therapeutic Strategies
Steroid Avoidance
Interests in corticosteroid abstention stems from the well-know side effects of osteoporosis, hyperglycemia, cushingoid features, hypertension, as well as the deleterious effects on recurrence of hepatitis C. The first randomized study concerning complete steroid avoidance was published by the Eason et al.
Renal Sparing Protocols
The sentinel articles by Ojo et al. and Gonwa et al. brought a stark realization about the true incidence of renal failure after transplant. Up to 21% of patients developed chronic renal failure within 5 years after receiving a nonrenal transplant.Thirteen years’ post–liver transplant, 18.1% of patients were diagnosed severe renal dysfunction, a significantly higher percentage when compared to controls.9 Both articles alluded to a direct role of CNIs.
Different strategies have been developed to help in this ongoing struggle. One approach has examined adding MMF and reducing the dose of the calcineurin inhibitor or eliminating the calcineurin inhibitor altogether. These studies have produced some encouraging results with up to 50% of patients showing at least a 15% improvement in renal function.
Conversion from CNI to Sirolimus
Recent studies with small numbers looked at the impact of switching patients with chronic renal impairment of CNI to RAP. Questions still remain on the optimal time to conversion and whether it can be used in the early posttransplant period. Large randomized trials are ongoing in an effort to answer these questions.
Calcineurin Inhibitor Avoidance
Very few studies have looked at complete calcineurin inhibitor avoidance. The latest data from the scientific registry of transplant recipients database show 99% of patients are discharged on either TAC (majority) or CyA. The concept of using agents without nephrotoxicity in solid-organ-transplant recipients where rejection has less of a negative impact on the long-term survival has sparked some enthusiasm, but to date little has been published to demonstrate success with this strategy.
Gastroenterol Clin North Am 1988;17:1-18; http://www.novartis-transplant.com/history/history_sandimmune.jsp;Drugs 1995;50:924-941; Transplant Proc 2004;36:2525-2531; Liver Transpl 2005;11:61-67;
Lancet 2000;355:376-377; Liver Transpl Surg 1999;5:502-508; Transplantation 2005;80:18-25. Read More......
Posted by Dr. E Flores Rivera at 11:20 PM 26 comments
Labels: immunosuppression, liver, transplantation
2006/09/15
Liver Regeneration
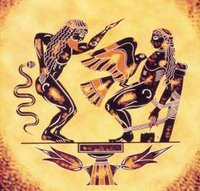 The earliest allusion to the liver’s regenerative capacity is described in Hesiod's Theogony (750-700 B.C.). A story about Prometheus, a Titan, who angered Zeus by stealing fire and giving it to the humans. As his punishment, Prometheus was chained to a rock in the Caucasus Mountains and tormented by an eagle, that each day flew to devour his liver. His damaged liver regenerated leaving him fit for the next days’ torture.
The earliest allusion to the liver’s regenerative capacity is described in Hesiod's Theogony (750-700 B.C.). A story about Prometheus, a Titan, who angered Zeus by stealing fire and giving it to the humans. As his punishment, Prometheus was chained to a rock in the Caucasus Mountains and tormented by an eagle, that each day flew to devour his liver. His damaged liver regenerated leaving him fit for the next days’ torture.Despite its large metabolic load, the liver is a largely quiescent organ in terms of cell proliferation, with only 0.01-0.001% of hepatocytes undergoing mitosis at any given time. This cellular turnover can be altered by toxic liver injury or surgical resection, which results in sudden, massive hepatocyte proliferation, producing recovery of functional liver mass within two weeks after the loss of up to two-thirds of the liver.
Experimental models of liver regeneration
Liver resection or partial hepatectomy (PH) reduces liver mass, but leaves few injured cells. Although the remaining hepatic segments are subjected to increased portal blood flow and pressure following PH, PH is still the closest approximation of pure liver regeneration unaccompanied by cellular injury and is therefore the preferred in vivo model to study.
Immediately following PH or other liver injury, hepatocytes exit the resting state of the cell cycle (G0), enter G1, traverse to DNA synthesis or S phase, and ultimately undergo mitosis, with a first peak of DNA synthesis occurring in the parenchymal cells (hepatocytes and bile duct epithelial cells). Non-parenchymal cells display a first peak of proliferation approximately 12-24 hours after the parenchymal cells. The degree of hepatocyte proliferation is directly proportional to the degree of injury, this being that any injury greater than about 10% will result in proliferation of cells throughout the liver.
Total liver mass is tightly modulated by pro-mitotic and apoptotic mechanisms, and possesses the remarkable ability to grow or shrink quickly in order to meet metabolic demands following hepatocellular injury or in response to situations of excess functional mass. An example of this is small-for-size liver transplants, where the liver will rapidly grow to accommodate the needs of the larger host, while larger livers transplanted into smaller hosts will undergo apoptosis to reach the normal liver to body mass ratio of 2.5%.
Although liver function appears virtually normal following PH, there can be no survival after liver injury without regeneration. In all animals studied, including humans, the failure to restore functional hepatic mass invariably leads to death. Impairment of liver regeneration is observed in some disease states (including non-alcoholic fatty liver disease, cirrhosis, chronic hepatic infection, malnutrition) with increased cell death, delayed mitosis and slower return of normal hepatic mass.
Intrinsic regenerative capacity of the liver
Serial transplant studies in mice suggest that the hepatocyte possesses an essentially limitless regenerative capacity, as shown by the works of Brinster and colleagues, and by Grompe.
In contrast to the impressive proliferative potential of the hepatocyte, the regenerative potential of the liver is limited. Clinical observations have determined that the upper-limit for single liver resection is approximately 70-80% in humans although if the functional liver mass returns to pre-resective levels, repeat resection of as much as 50% of the regenerated liver can be tolerated.
Evidence for the role of circulating factors in liver regeneration
 The realization that other organs and secreted factors are critical for the liver’s regenerative response began to be elucidated by Bucher, Starzl and others in the 1960s and 70s. Prior to that time the phenomenon of liver regeneration had been attributed to a flow-dependent response whereby increased relative flow following PH resulted in hepatocyte proliferation and hyperplasia. Bucher demonstrated the existence of "humoral factors" in the induction of liver growth following PH.
The realization that other organs and secreted factors are critical for the liver’s regenerative response began to be elucidated by Bucher, Starzl and others in the 1960s and 70s. Prior to that time the phenomenon of liver regeneration had been attributed to a flow-dependent response whereby increased relative flow following PH resulted in hepatocyte proliferation and hyperplasia. Bucher demonstrated the existence of "humoral factors" in the induction of liver growth following PH.Starzl and coworkers identified essential roles for several humoral factors, including islet cell-derived insulin along with an essential role for other gut-derived agents in dogs. This has resulted in the identification of factors involved in: 1) initiating or “triggering” the hepatic response to injury; 2) inducing hepatocyte proliferation; and 3) terminating cell proliferation once normal liver mass is restored have been identified.
Priming is accomplished by the release of preformed cytokines that subsequently activated transcription factor complexes and allow the cell to exit G0 to G1 of the cell cycle. After the priming event, increased expression of pro-mitogenic growth factors and their receptors is observed concomitant with down-regulation of hepatostatic factors and receptors. Facilitated by co-mitogens, growth factor signaling permits progression of the primed hepatocyte through the cell cycle.
Cessation of liver growth once normal mass is reached is also regulated by multiple pathways including increased expression and responsiveness to hepatostatic factors, or tonic growth inhibitors.
The secreted and soluble factors involved in the response to PH can be classified using the following five categories:
1) Priming Factors
2) Growth Factors
3) Co-mitogens
4) Tonic Growth Inhibitors
5) Suppressors of Growth Inhibitors
Tumor Necrosis Factor (TNF): TNF, a cytokine with pleiotrophic effects is required for normal liver regeneration. , TNF can induce DNA synthesis in cultured hepatocytes., as a priming agent which renders hepatocytes responsive to growth factors.
Interleukin-6 (IL-6): is a multifunctional proinflammatory cytokine involved in a variety of host defenses and pathological processes. IL-6 acts on the cell by binding the IL-6 receptor alpha chain (IL-6Ra, also known as gp80), inducing dimerization of the gp130 receptor and subsequent intracellular signaling partners. IL-6 is expressed both in the liver and the gut following liver resection.
Hepatocyte Growth Factor (HGF): HGF was isolated based upon its ability to induce DNA synthesis in cultured hepatocytes, but is now known to have pleiotrophic effects on many other tissues. Shown to weakly induce hepatocyte proliferation. Two reports of HGF transgenic mice, have led Fausto and others to postulate that normal hepatocytes in vivo have a low sensitivity to growth factors, and can only respond to such factors after gaining replicative competence by priming, or activation of the transcription factor complexes NF-kB, AP-1, and STAT3 followed by expression of immediate early genes.
Epidermal Growth Factor (EGF) and Transforming Growth Factor-alpha (TGF-): EGF stimulates the growth of various epidermal and epithelial tissues in vivo and in vitro, and of some fibroblasts in cell culture.
Insulin and Glucagon: Insulin is regarded as an anabolic, growth-promoting hormone, while glucagon has opposing activities, exerting a catabolic effect. Insulin and glucagon, particularly when administered together, have been shown to accelerate liver regeneration after PH.
Activin and Follistatin: Activin, another member of the TGF-ß superfamily, has potent growth inhibitory effects on hepatocytes
Chemokines: a diverse group of approximately 30 known members involved in a wide variety of inflammatory processes. Chemokines have been shown to facilitate recovery following toxic liver injury, and may play a role in regulating hepatocyte proliferation either directly, or indirectly through induction of HGF expression.
Prostaglandins: PGE2, prostacyclin, and thromboxane, may be involved in growth regulation after PH. Prostaglandins are synthesized from arachidonic acid released from membrane phospholipid by phospholipase A2. Arachidonic acid is oxidized by cycloxygenases (COX) to generate the precursor PGH2, which is further metabolized to form prostaglandins, thromboxanes, and prostacyclins. Although COX inhibitors have not yet been demonstrated to block regeneration in humans, these data suggest that care should be exercised in the use of non-steroidal anti-inflammatory agents, such as indomethacin, following major liver resection.
Steroids and Thyroid Hormone: steroids have been noted to regulate both cell growth as well as fatty content of hepatocytes. Sex steroids are known to induce transient hepatocellular proliferation and improve fatty acid metabolism. Pre-treatment of rats with 17ß-estradiol induces hepatocyte DNA synthesis in vitro and accelerates liver regeneration in vivo. Thyroid hormone (T3) is also a powerful inducer of hepatocyte proliferation in vitro and in vivo.
Glucocorticoids inhibit hepatocyte proliferation as well as decrease the expression of a number of the genes involved in fatty acid metabolism. Thus the use of glucocorticoids may impair liver regeneration both by aggravating steatosis and inhibiting growth.
Intracellular signals involved in liver regeneration
Identified over 200 genes associated with signaling processes in addition to the many hundreds of genes also being expressed and modulating the regenerative response.
Priming Pathways:
TNF Receptor Signaling: TNF renders the hepatocyte competent to respond to growth stimuli.
Nitric Oxide: highly reactive molecule synthesized from arginine by nitric oxide synthase (NOS). Three distinct isoforms of NOS exist, constitutive NOS (cNOS) (which includes brain (bcNOS) and endothelial NOS (ecNOS)) and inducible NOS (iNOS). In the case of compensatory hepatic growth both the cNOS and iNOS isoforms are thought to play a critical role in successful hepatic regeneration following PH.
It appears that iNOS induction occurs predominantly in the hepatocytes and coincides with the pre-cell replication phase (6-8 hours). The induction of iNOS is cytokine dependent and has been demonstrated to coincide with the induction of IL-6 inducible transcription factors. NO plays an essential role on hepatocyte repopulation of the liver.
Growth Promoting Pathways: Sub-divided into four groups: guanine nucleotide protein (G-protein) coupled-receptors, receptors with intrinsic tyrosine kinase activity, receptors that recruit cytoplasmic kinases, and nuclear hormone receptors. When activated subtypes result in expression of growth related genes. essential for cell proliferation.
Growth-Inhibitory Pathways: Cessation of liver growth after regeneration and indeed perhaps the tonic growth-inhibition of the liver in the normal state is at least partly mediated by the TGF-ßs and the Activins, all members of the TGF-ß superfamily. Recent evidence suggests that TGF-ß/Activin signaling in early liver regeneration might be blocked by increased expression of the Smad pathway inhibitors SnoN and Ski.
Interactions of signaling pathways during liver regeneration
The presence of numerous diverse yet specific ligands and receptors in the initiation, propagation and termination of the process of hepatic regeneration is an essential factor in the successful and complete restoration of hepatic mass. But, hepatic regeneration cannot proceed unless the activated receptors each communicate successfully with the cell nucleus to allow the regulation of transcriptional factors and subsequent de novo DNA synthesis, cell proliferation and differentiation. Receptor activation and regulation of intracellular pathways represent common means by which distinct receptors can communicate with the nucleus, and are laid out as linear signal transduction pathways.
Apoptosis during liver regeneration
Initiation of proliferation may be difficult or impossible for certain diseased hepatocytes. Cell death under these circumstances will occur by a process of preprogrammed cell death, termed apoptosis. In vivo apoptosis may be activated by engagement of the socalled "death receptors" by their ligands, including Fas ligand, which is a protein secreted by lymphocytes, TNF, and TNF-related molecules or by activation of serine-threonine kinase receptors by members of the TGF-ß superfamily, including Activin and TGF-b.
Alternatively, apoptosis may be activated secondarily to mitochondrial release of cytochrome C after drug-induced injury. During activation, a number of caspase enzymes and intracellular signals of the bcl2 family (Bad, Bak, Bax) become activated. In turn, these lead to digestion of the nucleus and destruction of the cell’s DNA, primarily through the direct action of caspase 3. During successful liver regeneration, the expression and activity of pro-apoptotic pathways is inhibited through increased expression of anti-apoptotic Bcl-2 family members (notably Bcl-2 and Bcl-XL).
Numerous factors have been implicated in activating anti-apoptotic signals in the liver inducible nitric oxide synthase and IL-6. Certain disease states lead to an impaired ability to down regulate apoptotic pathways in the liver, like steatosis, for example. Ischemic preconditioning, i.e. providing a short period of ischemia followed by reperfusion of the liver prior to undergoing liver resection, has been shown both in animal and human studies to decrease apoptosis associated with liver resection both in hepatocytes as well as in hepatic endothelial cells.
Ischemic preconditioning has been demonstrated to decrease post-resective serum markers of liver injury in both animal and human studies. This phenomenon is even more pronounced if steatotic liver is treated. Clavien and coworkers demonstrated success in humans undergoing liver resection with an ischemic preconditioning protocol involving 10 minutes of ischemia followed by 10 minutes of reperfusion prior to hepatic resection. The pathways that elicit this protective response are still under active investigation, although work by Diehl and colleagues and Jaeschke et al. implicates nitric oxide, TNF, and neutrophils in the oxidant and protease-mediation of hepatocellular injury after experimental ischemia/reperfusion injury.
Effects of steatosis, steatohepatitis, fibrosis and cirrhosis on liver regeneration
 Data from clinical centers that perform hepatobiliary surgery and living donor transplantation report a typical operative mortality of less than 2-3% associated with major liver resection when performed on normal liver. In the presence of underlying steatosis the associated operative mortality has been noted to be as high as 10%.
Data from clinical centers that perform hepatobiliary surgery and living donor transplantation report a typical operative mortality of less than 2-3% associated with major liver resection when performed on normal liver. In the presence of underlying steatosis the associated operative mortality has been noted to be as high as 10%.Steatohepatitis is therefore a relative contraindication to major hepatic resection or use for transplantation. Mortality following resection in these livers generally occurs within days after surgery when regeneration fails and liver failure and hepatocyte apoptosis occurs. Whole organ liver abnormalities that result from steatosis include reduction of the sinusoidal space, which in turn may result in abnormal blood flow. Lipid accumulation is also associated with hepatocyte mitochondrial damage. This is due to free radical injury from abnormal fatty acid oxidation and accumulation of dicarboxylic fatty acids during intermediary metabolism. Abnormalities in cytochrome p450 (CYP) induction have also been implicated in fatty liver and steatohepatitis.
Hepatic fibrosis, biochemically, represents the partially reversible accumulation of a fibrillar collagen matrix and relative loss of the normal type IV collagen matrix basement membrane. This phenomenon has been found to begin in the subendothelial space and is due largely to the secretion of abnormal collagen by stellate cells. Abnormal regeneration is manifest in the fibrotic liver due to the chronically impaired diffusion of nutrient and hepatotrophic factors through the abnormal fibrillar basement membrane. Impaired hepatocyte function results from absence of normal trophic factors. Furthermore, the scar contracture of cirrhosis also becomes a physical barrier to compensatory hyperplasia following resection.
Effects of commonly prescribed drugs on liver regeneration
Effects of various medications on liver regeneration have become recognized. Of particular concern are herbal supplements, which contain numerous, often poorly-defined biochemicals including numerous agents that may stimulate nuclear receptors to induce steatosis or even NASH. Cessation in patients about to undergo liver resection is suggested.
Beta-blockers inhibit the effects of epinephrine, an important comitogen for hepatocytes. They also decrease portal flow and, as such, have a critical role in the management of portal hypertension. The cellular mechanism involves decreased G-protein coupled signaling with impaired adenylate cyclase, cAMP and down-stream signals. reduction of portal blood flow may restrict the perfusion of enterically-derived factors such as TNF and EGF into the liver.
J Gastroenterol Hepatol 1996; 11:466–470; Arch Surg 2000;135:1353–1358; Semin Liver Dis 2002;22:137–144; Radiology 1999;210:467–477; J Surg Res 2001;96:289–295; Liver Transplant Surg 1996;2:233–234; Hepatology 1991;13:1–5; J Hepatol 1996;24:385–390; Hepatology 1994;19:489–497; Hepatology 2003;38:326–334; Ann Surg 2002;235:863–871.
Posted by Dr. E Flores Rivera at 5:26 PM 0 comments
Labels: liver, regeneration